Cognitive Rehabilitation (3) - Assessment of Cognitive Processes
(29/11/2022)
"There is no thing that is not made easier through
constancy and familiarity and training.
Through training we can change;
we can transform ourselves."
(Fourteenth Dalai Lama Tenzin Gyatso)
In the previous article we described some possible cognitive consequences of a brain injury, with references to historical, clinical, or experimental cases; today we will begin to talk more specifically about the rehabilitation therapy that aims to counteract these situations by stimulating and rebalancing the activity and function of our brain as much as possible: cognitive rehabilitation. We will divide this wide topic into two parts and talk today about how a person's cognitive abilities can be assessed. We will also make some remarks about the importance of video game scenarios included in this type of pathways.

As reported by Novakovic-Agopians and Abrams [«Cognitive Rehabilitation Therapy» Encyclopedia of the Neurological Sciences (2nd Edition), 2014], cognitive rehabilitation therapy has been defined by the American Congress of Rehabilitation Medicine as a systematic, functional cognitive therapeutic activity oriented toward achieving functional changes:
- by re-establishing or reinforcing previously learned patterns of behavior,
or
- by establishing new patterns of cognitive activity or compensatory mechanisms for impaired neurological systems.
Cognitive rehabilitation is similar to other types of rehabilitation therapy and includes both restorative and compensatory approaches.
- Restorative therapy is based on the principle that repetitive exercise of the neural circuits that mediate cognitive function leads to the learning of new skills, which will reverse the deterioration caused by the injury. This type of treatment assumes that the surviving or unimpaired neural tissue is able to reorganize itself (neuroplasticity) to replace the lost function.
- Compensatory therapy, on the other hand, is based on the avoidance of mechanisms that were previously necessary for a specific skill. By substituting functional pathways, or using adaptive techniques or equipment, alternative methods are learned to achieve the desired goal.
Separating restorative and compensatory training is difficult because the cognitive processing practiced during compensatory therapy can stimulate the neural pathways that mediate new learning.
What are the most modern tools used by Sector Professionals?
Nowadays, “robotic medical devices for rehabilitation” are commonly used: these devices are particularly used for precise therapies supported by high-tech systems that can help the Therapist to set repetitive, intense and task-specific exercises. A considerable number of these technologies are dedicated to neuromotor rehabilitation following stroke, so much so that we now often hear of highly specialized facilities that offer “robotic rehabilitation” pathways or are equipped with gyms for “technologically assisted treatments”. But how does this topic dovetail with that of cognitive rehabilitation?
Indeed, one type of rehabilitation approach that is becoming increasingly popular involves using these robotic devices precisely to set up cognitive training as well. After all, it turns out intuitively that the possibilities offered by a certain technology are many, so it was a matter of time before it was decided to try to expand the use of rehabilitation robots by combining the demand for motor-type performance with others of a more cognitive nature, or even by differentiating them more according to the purpose and needs of patients.
Thus, a robotic device for rehabilitation can also be used to administer cognitive therapeutic treatments to patients who need this type of approach.
There are also devices that propose the use of immersive Virtual Reality environments or specific software applications to set up cognitive rehabilitation treatment. We will return on these topics later.
Let us now return to the central topic of this article and reflect on setting up a cognitive training or rehabilitation pathway, for example, for patients suffering the consequences of a neurological trauma (such as a stroke) or suffering from decline due to a degenerative disease or brain injury.
The first question a Therapist should ask before establishing the characteristics of a cognitive rehabilitation treatment is, “What are my Patient's cognitive abilities?” This is true in both the motor and cognitive domains: each session, in fact, should be established and customized based on the abilities and needs of the patient or subject being treated.
Result (rather negative) of the "Brain Age Test" in the educational video game "Dr. Kawashima's Brain Training" developed for Nintendo Switch. ©Nintendo, 2020
A valuable cognitive screening tool is the Italian version of the Oxford Cognitive Screen (OCS), recently developed with the specific aim of describing cognitive deficits after stroke [«The Oxford Cognitive Screen (OCS): Validation of a stroke-specific short cognitive screening tool» Psychological Assessment, 2015], [«Italian normative data for a stroke specific cognitive screening tool: the Oxford Cognitive Screen (OCS)» Neurological Sciences, 2016].
This scale consists of 10 tasks that include five cognitive domains: attention and executive functions, language, memory, number processing, and praxis (we discussed these cognitive domains in a previous article). Also included is a brief assessment of visual field defects.
The following are examples of Tests that are useful for conducting a cognitive assessment of a patient who has suffered a brain injury.
- Symbol and digit association test (attention and processing speed).
The subject is shown a page in which, in the first line, nine symbols are associated "one by one" with as many digits, from 1 to 9. The rows below contain only symbols, and subjects are required to orally report the digit associated with each symbol. The number of correct responses in 90 seconds is measured. A higher score indicates higher cognitive functions [«Symbol digit modalities test», Los Angeles, 1973], [«The symbol digit modalities test - Oral version: Italian normative data» Functional Neurology, 2006].
- Task of storing a list of digits (memory).
The “Digit span forward” task originally suggested by Hebb is proposed [«Distinctive features of learning in the higher animal» Brain Mechanisms and Learning, A Symposium, 1961]. The examiner pronounces a list of digits, at a rate of about one per second, and asks the subject to repeat it immediately in the same order. If successful, a list containing one more digit is presented. If the subject fails to perform the task, a second list of the same length is presented. If the subject succeeds with the second list, a list one digit longer is presented, as described earlier. However, if one also fails with the second list, the test is terminated. The length of the digit sequences increases gradually, starting from a sequence of three numbers (e.g., 5, 8, 2) to a sequence of up to nine (e.g., 7, 1, 3, 9, 4, 2, 5, 6, 8). The span is established as the length of the longest list correctly retrieved [«Forward and backward span for verbal and visuo-spatial data: Standardization and normative data from an Italian adult population» Neurological Sciences, 2013].
- Rey-Osterrieth complex figure (visuospatial skills and visual memory).
The test, originally designed by Rey [«L’examen psychologique dans les cas d’encéphalopathie traumatique» Archives de Psychologie, 1941] and later standardized by Osterrieth [«Le test de copie d’une figure complexe; contribution à l’étude de la perception et de la mémoire» Archives de Psychologie, 1944], requires the subject to copy a complex geometric figure (the condition is to make an immediate copy) [«Clinical and empirical applications of the Rey-Osterrieth Complex Figure Test» Nature Protocols, 2006]. Regarding the test, performance accuracy is calculated by applying the standard scoring criteria, in which the geometric figure is divided into 18 units and rated on a 2-point scale for both accuracy and placement [«Complex Figure Test and recognition trial professional manual» Psychological Assessment Resources, 1995].
- Tower of London (executive functions).
This is a useful neuropsychological tool for measuring planning and problem-solving skills [«Specific impairments of planning» Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 1982], [«Planning abilities and the Tower of London: is this task measuring a discrete cognitive function?» Journal of Clinical and Experimental Neuropsychology, 2004], [«The Tower of London spatial problem-solving task: Enhancing clinical and research implementation» Journal of Clinical and Experimental Neuropsychology, 2002], [«The Tower of London (ToL) in Italy: standardization of the ToL test in an Italian population» Neurological Sciences, 2017]. Briefly, this test consists of a board with three vertical sticks of different (increasing) lengths in which three different colored wooden balls are placed. The shortest stick houses one ball, the second two and the third three. Subjects are shown a certain configuration of balls within the sticks and a picture of the final configuration. Subjects are then required to move the balls to reach the final configuration, provided they do not break certain rules (each stick can accommodate a different number of balls, only one ball can be moved at a time, balls cannot be placed outside the sticks, and a maximum number of movements are allowed). Three scores are calculated for this test: points, time (measured as the sum of "planning" time and "execution" time), and errors.
- Stroop test for colors and words (executive functions).
It is a neuropsychological instrument widely used in clinical practice to assess selective attention, cognitive flexibility and sensitivity to interference, skills related to the frontal lobes. Three tasks are proposed in the short version of this test [«A short version of the Stroop test: Normative data in an Italian population sample» Nuova Rivista di Neurologia, 2002]:
- word - (word reading): 3 lists of 10 words (“red”, “blue”, “green”) are given in random order to patients, each written in black ink; they must read the written words;
- color - (color naming): 3 lists of 10 colored circles (red, blue, green) are given in random order to patients; they must name the color of the circles;
- color-word (interference test): 3 lists of 10 words (“red”, “blue”, “green”), each written in colored ink (red, blue or green) different from the color name indicated by its meaning and in all possible combinations, are offered to patients in random order and they are asked to name the color of the ink used to write each word, not the word itself.
For each test, the running time (T1, T2, T3) and any errors committed are recorded. Two interference effects are then calculated and used as results: time (difference between the time spent in the third test and the average time spent in the previous two tasks), and error (difference between the number of errors made in the third test and the average time spent in the previous two tasks).
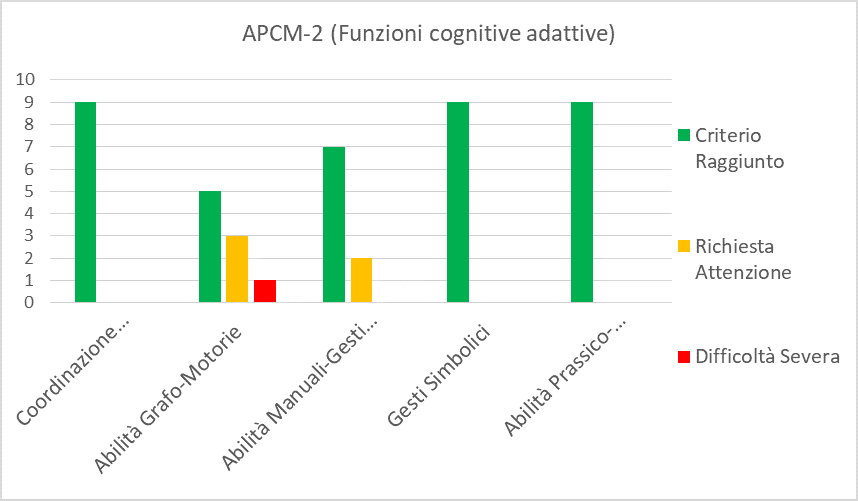
Example of a chart showing the assessment of some cognitive skills (written in Italian)
Once a patient's “cognitive abilities” have been established, it will then be possible to set up a specific treatment, defining exercises and goals for stimulation and rehabilitation.
We can now make a connection to the topic mentioned at the beginning of this article, namely robotic devices and Virtual Reality scenarios currently used in rehabilitation.
Speaking of the most modern robotic devices for rehabilitation, we have seen that there is extensive use of seemingly video-ludic scenarios to set up exercises. This fact may seem almost “strange” to a layman, since today's older people are generally unfamiliar with the world of “video games” or interactive Virtual Reality scenarios shown on a screen or through a visor. What, then, is the rationale behind this kind of approach?
In recent years, there has been a growing hypothesis that video games can promote specific modifications in certain areas of the nervous system. Because of their characteristic ability to engage, as we have seen, video games are also being offered to neurological patients not for recreational purposes, but for therapeutic purposes in order to make rehabilitative therapies more stimulating and intense (this is precisely what is referred to as Serious Games). An international authority in the field of videogaming for the purpose of cognitive stimulation is Ryuta Kawashima, a Japanese Physician and Neuroscientist and Full Professor at Tohoku University.
A 2019 review, which mainly analyzed 3D adventure, first-person shooting (FPS), puzzles, rhythmic dancing and strategy tasks, shows that video games affect brain structure and function depending on how the game is played. The results of this article showed that video games can be beneficial to our brains, although the beneficial effects vary depending on the type of video game [«Does Video Gaming Have Impacts on the Brain: Evidence from a Systematic Review» Brain Sciences, 2019].
Cognitive stimulation through gaming has also been shown to be a method for enabling the maintenance of a healthy brain and limiting the decline in cognitive function necessary to perform daily activities in older adults with dementia [«Designing Serious Computer Games for People With Moderate and Advanced Dementia: Interdisciplinary Theory-Driven Pilot Study» JMIR Serious Games, 2017].
In fact, research has found that even the elderly (not just the young) can be Serious Games players [«Clinical trial design of serious gaming in mild cognitive impairment» Frontiers in Aging Neuroscience, 2015]. In this regard, there is strong empirical evidence that video games and online activities have beneficial effects on cognitive functioning in the elderly even with dementia in several areas such as: reaction time, memory, attention span, control of cognitive function, and increased multitasking abilities [«Video Games and Other Online Activities May Improve Health in Ageing» Frontiers in Medicine, 2018]. Here's why, compared to last decade, today's elderly are increasingly video game users [«Recommendations for the use of Serious Games in people with Alzheimer’s Disease, related disorders and frailty» Frontiers in Aging Neuroscience, 2014].
Thus, it does not seem contraindicated (in fact, far from it) to use a mechanical or robotic device combined with Serious Games with patients who have cognitive as well as motor difficulties.
Having ascertained that the course of cognitive rehabilitation should be established taking into account neuropsychological and neurological evaluations, also comparing with other professional figures such as the speech therapist (especially in the case of speech disorders), with the tools listed so far we will be able, in the next article, to analyze some types of exercises that are actually proposed to patients who need to recover certain abilities. Just as a person with weak quadriceps femoris will be asked to do certain lower limb exercises, a patient with aphasia may do exercises of a linguistic nature, or in the case of spatial eminegligence, tasks of exploring the surroundings will be suggested. It is clear that analyzing all the possibilities of cognitive training would open up a vast and, as we have seen, extremely complex world; however, we will try to outline the practical approach, the method of setting with some examples taken from real rehabilitation contexts. We will also continue to give ample space to what are software or hardware tools currently used precisely in the cognitive rehabilitation branch.